
HYDRATE AND NOURISH DYSPHAGIC PATIENTS
Food for special medical purposes suitable for the dietary management of patients with difficulty in swallowing (dysphagia),difficulty in swallowing liquids and in chewing, thus requiring a diet of an appropriately modified consistency.
- Gelling powders for water and beverages
- Thickeners for liquid and semi-liquid foods
- Ready to use gelled beverages
Dysphagia Products
-
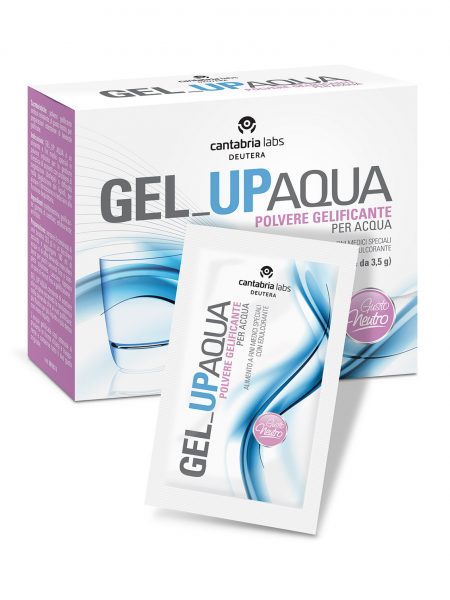
GEL_UP AQUA
70 g box (20 sachets of 3.5 g each) -
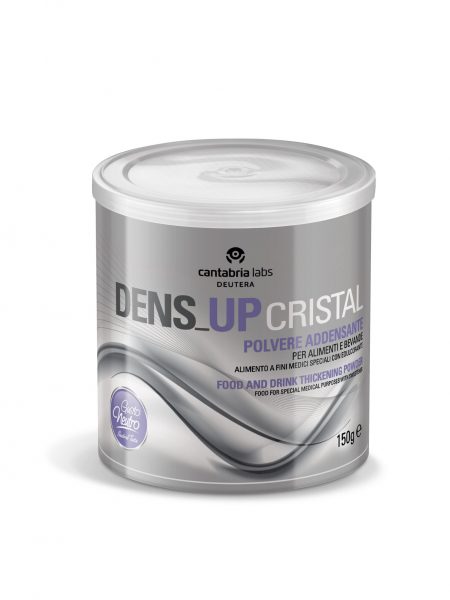
DENS_UP Cristal
250 g and 150 g jar with 5 ml measuring scoop, equivalent to approximately 2 g of powder -

VALBLAN
Pack of 24 jars of 125 g each. -
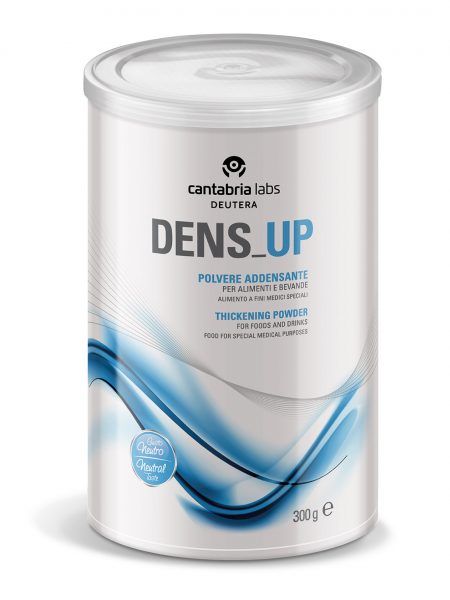
DENS_UP
300 g and 500 g jar with 10 ml measuring scoop, equivalent to 3.5 g of powder -
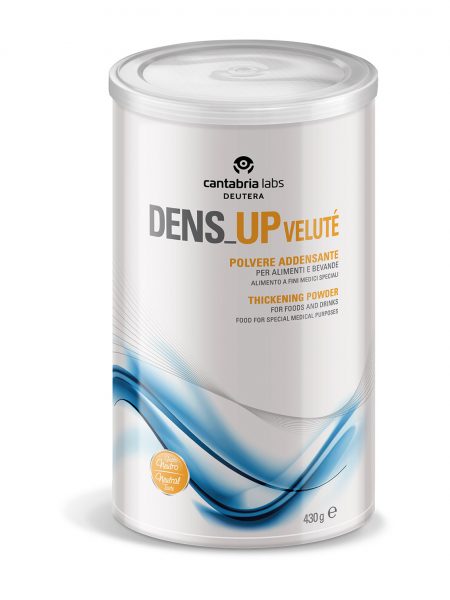
DENS_UP Velutè
430 g jar with 10 ml measuring scoop, equivalent to approximately 2.5 g of product
0
0
Cart
Empty CartShop
![]()
Spedizione gratuita per ordini
superiori ai 47 €.
Tutti i costi dei prodotti sono IVA inclusa.
| Nutritional Info | Average Analysis | |
|---|---|---|
| for 100 g | for 1 measuring scoop (2,5 g) | |
| Energy | 1609 kJ | 40,2 kJ |
| 379 kcal | 9,4 kcal | |
| Fat | < 0,5 g | 0 g |
| of which saturates | < 0,1 g | 0 g |
| Carbohydrate | 94,8 g | 2,3 g |
| of which sugars | 0 g | 0 g |
| of wich starch | 94,8 g | 2,3 g |
| Fibre | 0,5 g | 0 g |
| Protein | < 0,1 g | 0 g |
| Salt | 0,5 g | 0 g |
Sconto quantità se acquisti almeno 12 articoli hai diritto ad uno sconto del 33% sul totale del carrello. Puoi acquistare anche un articolo per prodotto, l'importante è che il totale nel carrello sia di 12 articoli
